Despite some wins, the transition to EHRs has generally been much slower than we anticipated, much harder than we imagined, and it is not hard to argue that interoperability of granular health data remains frustratingly elusive.
"Smart data, smarter healthcare"
Bridging the interop chasms
Case Study: Clinical Engagement
Bridging the gap between the clinical experts and software engineers involved in eHealth projects is well known for being difficult and frustrating for both sides. The openEHR methodology is having great success in bringing the non-technical clinicians along with us on the clinical modelling journey.
Take off the low-res sunglasses
Clinical modelling, openEHR style
The outcome of a program of coordinated clinical content standardisation provides a long term and sustainable national approach to developing, maintaining and governing jurisdictional health data specifications. It can form the backbone for a national health data strategy and is a key way to ensure that clinicians contribute their expertise to jurisdictional eHealth programs.
The Archetype 'Elevator Pitch'
Standards Development?
https://twitter.com/psujorge/status/438909282499977216
Technical/Wire...Human/Content
In a comment on one of my most recent posts, Lloyd McKenzie, one of the main authors of the new HL7 FHIR standard made a comment which I think is important in the discourse about whether openEHR archetypes could be utilised within FHIR resources. To ensure it does not remain buried in the rather lengthy comments, I've posted my reply here, with my emphasis added.
Hi Lloyd,This is where we fundamentally differ: You said: "And we don’t care if the data being shared reflects best practice, worst practice or anything in between."
I do. I care a lot.
High quality EHR data content is a key component of interoperability that has NEVER been solved. It is predominantly a human issue, not a technical one - success will only be achieved with heaps of human interaction and collaboration. With the openEHR methodology we are making some inroads into solving it. But even if archetypes are not the final solution, the models that are publicly available are freely available for others to leverage towards 'the ultimate solution'.
Conversely, I don't particularly care what wire format is used to exchange the data. FHIR is the latest of a number of health data exchange mechanisms that have been developed. Hopefully it will be one that is easier to use, more widely implemented and will contribute significantly to improve health data exchange. But ultimately data exchange is a largely technical issue, needs a technical solution and is relatively easy to solve by comparison.
I'm not trying to solve the same problem you are. I have different focus. But I do think that FHIR (and including HL7 more broadly) working together with the openEHR approach to clinical modelling/EHRs could be a pretty powerful combo, if we choose to.
Heather
We need both - quality EHR content AND an excellent technical exchange format. And EHR platforms, CDRs, registries etc. With common clinical archetypes defining the patterns in all of these uses, data can potentially start to flow... and not be blocked and potentially degraded by the current need for transforms, mappings, etc.
Stop the #healthIT 'religious' wars
I seemed to trigger an interesting discussion over on Grahame Grieve's blog when I posted the following question to him on Twitter. https://twitter.com/omowizard/status/432869451739185152
Grahame responded a la blog, but not really answering the essence of my question.
However, below is a great comment copied directly from the discussion thread, and submitted by Koray Atalag (from openEHR NZ). In it he has succeeded in expanding my twitter-concise thoughts rather eloquently:
"Hi guys,
I’m interested in getting these two awesome formalisms as close as possible. In what way – have no clue at the moment apart from existing mutual understanding and sympathy at a personal level. Well that’s where things start I guess
Ed Hammond once said, as he was visiting us in Auckland last year, convergence in standards is a must, mappings just become complex and hard to maintain. I kind of agree with that. Where I’d like to see openEHR and FHIR is really dead simple – Share what they are the best. Here is how I see things (and apologise if you find too simplistic): 1) Archetypes are THE way to model clinical information – anyone argue with that? 2) FHIR IS the way to exchange health information over the wire; modern, non-document/message oriented, heaps of interest from vendors etc. 3) openEHR’s Model Driven Development methodology can be used to create very flexible and highly maintainable health information systems. So this is a different territory that FHIR covers. Inside systems vs. Outside. A growing number of vendors have adopted this innovative approach but it’d be dumb to expect to have any significant dominance over the next decade or so.
So why not use openEHR’s modelling methodology and existing investment which includes thousands of expert clinicians’ time AND feed into FHIR Resource development – I’d assume Archetypes will still retain lots of granularity and the challenge would be to decide which fall under the 80%. I take it that this proportion thing is not mathematical but a commonsense thingy.
As with anything in life there is not one perfect way of doing health IT; but I feel that FHIR based health information exchange with propriety (and from the looks increasingly monolithic) large back-end HIS and openEHR based health information systems working with rich and changeable clinical data (note some Big Data flavour here
will prevail in this rapidly changing environment.
So I’m interested – probably mapping as a starting step but without losing time we need to start working together.
The non-brainer benefits will be: 1) FHIR can leverage good content – I tend to think a number of Published or Under Review type archetypes have been in use in real life for a while and that’s probably what Heather was referring to by clinical validation. A formal clinical validation is a huge undertaking and absolutely unnecessary I guess unless you’re programming the Mars Colonisation Flight health information systems!
2) openEHR can learn from FHIR experience and use it as the means to exchange information (I haven’t yet seen EHR Extracts flying over using modern web technologies). There is an EHR service model and API but I’d say it is not as mature as rest of the specs.
3) Vendors (and the World for that matter) can benefit from 1) mappings; and then 2) better FHIR Resources in terms of more effectively managing the semantic ‘impedance mismatch’ problem. An example is medication – I’d assume an HIS data model for representing medication should have at least the same granularity as the FHIR Resource it ought to fill in (practically only the mandatory items). If any less you’re in trouble – but having a sound model will ease the HIS internal data model matching and help with deciding which part is 80% vs. 20%.
4) Needless to say vendors/national programmes using pure openEHR vs. FHIR + something else will benefit hugely. Even ones using CDA – remember some countries are using (or just starting as in New Zealand) Archetypes as a reference library and then creating payload definitions (e.g. CDA) from these. So having this openEHR – FHIR connection will help transition those CDA based implementations to FHIR. Interesting outcome
5) I think in the long run vendors can see the bigger picture around dealing with health information inside their systems and perhaps start refactoring or rebuilding parts of it; e.g. clinical data repositories. An HIS with sound data model will likely to produce better FHIR instances and definitely have more capability for using that information for things like advanced decision support etc.
All for now…"
And then the conversation continues, including Thomas Beale from @oceaninfo and Borut Fabjan from @marandlab. I know of many others who have expressed a strong desire for openEHR clinical content and FHIR to be more aligned and collaborative.
FHIR seems here to stay - it is gathering fantastic momentum. The openEHR methodology for developing clinical content is also gathering momentum, including national program adoption in a number of countries and in clinical registries.
Chuck Jaffe (CEO of HL7) emphasised the need for collaboration between standards at last week's Joint Inter-Ministerial Policy Dialogue on eHealth Standardization and Second WHO Forum on eHealth Standardization and Interoperability at the World Health Organisation in Geneva.
So let's do it.
We all live in the real world and need to be more proactive in working together.
It is time to stop the 'religious wars', especially the long-time, tedious 'not invented here' argument between openEHR and HL7 and the ever-ongoing lets 'reinvent the wheel' approach to EHR content that occurs more broadly.
I call on all participants in the eHealth standards world to get the 'best of breed' standards working together.
Oil & water: research & standards
The world of clinical modelling is exciting, relatively new and most definitely evolving. I have been modelling archetypes for over 8 years, yet each archetype presents a new challenge and often the need to apply my previous experience and clinical knowledge in order to tease out the best way to represent the clinical data. I am still learning from each archetype. And we are still definitely in the very early phases of understanding the requirements for appropriate governance and quality assurance. If I had been able to discern and document the 'recipe', then I would be the author of a best-selling 'archetype cookbook' by now. Unfortunately it is just not that easy. This is not a mature area of knowledge. I think clinical knowledge modellers are predominantly still researchers.
In around 2009 a new work item around Detailed Clinical Models was proposed within ISO. I was nominated as an expert. I tried to contribute. Originally it was targeting publication as an International Standard but this was reduced to an International Specification in mid-development, following ballot feedback from national member bodies. This work has had a somewhat tortuous gestation, but only last week the DCM specification has finally been approved for publication - likely to be available in early 2014. Unfortunately I don't think that it represents a common, much less consensus, view that represents the broad clinical modelling environment. I am neither pleased nor proud of the result.
From my point of view, development of an International Specification (much less the original International Standard) has been a very large step too far, way too fast. It will not be reviewed or revised for a number of years and so, on publication next year, the content will be locked down for a relatively long period of time, whilst the knowledge domain continues to grown and evolve.
Don't misunderstand me - I'm not knocking the standards development process. Where there are well established processes and a chance of consensus amongst parties being achieved we have a great starting point for a standard, and the potential for ongoing engagement and refinement into the future. But...
A standards organisation is NOT the place to conduct research. It is like oil and water - they should be clearly separated. A standards development organisation is a place to consolidate and formalise well established knowledge and/or processes.
Personally, I think it would have been much more valuable first step to investigate and publish a simple ISO Technical Report on the current clinical modelling environment. Who is modelling? What is their approach? What can we learn from each approach that can be shared with others?
Way back in 2011 I started to pull together a list of those we knew to be working in this area, then shared it via Google Docs. I see that others have continued to contribute to this public document. I'm not proposing it as a comparable output, but I would love to see this further developed so the clinical modelling community might enhance and facilitate collaboration and discussion, publish research findings, and propose (and test) approaches for best practice.
The time for formal specifications and standards in the clinical knowledge domain will come. But that time will be when the modelling community have established a mature domain, and have enough experience to determine what 'best practice' means in our clinical knowledge environment.
Watch out for the publication of prEN/ISO/DTS 13972-2, Health informatics - Detailed clinical models, characteristics and processes. It will be interesting to observe how it is taken up and used by the modelling community. Perhaps I will be proven wrong.
With thanks to Thomas Beale (@wolands_cat) for the original insight into why I found the 13972 process so frustrating - that we are indeed still conducting research!
Engaging clinicians: building EHR specifications
There is a methodology that is pragmatically evolving from my experience in openEHR clinical modelling work over the past few years. It has developed in a rather ad hoc way, and totally in response to working directly with clinicians. The simplicity and apparent effectiveness – both for me and the clinicians involved - continues to surprise me each time I use it. The clinical content specifications for specialised health records and care plans that we are building are being developed with a sequence of expert input and clinical verification:
- Identifying the clinical requirements and business rules in conjunction with a selected initial domain expert group;
- Broader abstract verification of the notion of ‘maximal data set’ for ‘universal use case’ during formal archetype review cycles;
- Contextual validation during template review by ‘on-the-ground’ clinicians; and finally, although to a lesser degree,
- Validation during mapping and migration of legacy data.
With each project I am refining this process. Starting off a project with face-to-face meetings has been a ‘no brainer’ – after all, it takes a while for everyone to understand the get the idea of what we are doing. However after initial workshops, pretty much everything else can be done via web conference, online collaboration via CKM and email.
I find the initial workshops are usually greatly satisfying. Within hours we can be creating two outputs – a mind map that reflects the clinicians evolving conversation about their requirements and, in parallel, an equally agile template of clinical content specifications that can be verified by the clinicians in real time.
The mind map is displayed on a shared screen or via a data projector and acts as a living document, evolving as we talk through the clinical requirements, and identify the complexities, dependencies and relationships of all the components. The final mind map may be surprisingly different to how it started, and at the end of the conversation, the clinicians can verify that what they’ve said if accurately reflected in the mind map. It is an open source tool, so we can also share this around after the workshop for further comments.
Most recently I have begun building a template on the fly during the workshop, using any existing archetypes that are available, and identifying gaps or the need for new archetypes on the mind map as we go. In this way we are actually building the content specification in front of the clinicians as well. They get an understanding of how the abstract discussion will actually shape the resulting EHR content and they can verify it as we gradually pull it together. The domain experts are immediately equipped to answer the question: “Does this specification match what you have been telling me you do in practice?”
This methodology seems to bring the clinicians along with us on the clinical modelling journey, and most are able to understand at least some of the implications of some of our requirements discussions and, in particular, the ‘shape’ of the data that we can collect. It is a process seems to suit the thinking process of many clinicians and the overwhelmingly consistent feedback from recent workshops is that they have all actually enjoyed the experience and want to know what are the next steps for them to be involved. So that’s certainly a winner.
And the funders/jurisdictions are anecdotally confirming for me that they are finding that this approach is supporting higher quality specifications in a much shorter time frame.
For example, at a project kickoff workshop for a new project recently, in two days we:
- developed a series of mind maps capturing a consensus view of the clinical requirements and business processes;
- identified all the archetypes required for the entire project, including those that existed and were ‘fit for use’, those that needed some extension to meet requirements and new archetypes that needed to be created;
- identified sources of information or mind mapped the requirements for each new archetype identified; and
- built 3 templates comprising all of the existing archetypes available from a number of sources – the NEHTA CKM http://dcm.nehta.org.au/ckm/, the openEHR international CKM http://www.openehr.org/ckm/ and local drafts that I had on my own computer. For a number of the new archetypes we also collectively identified source information that would inform or be the basis for the archetype development.
All of this described above took 8 medical practitioners clinicians away from their everyday practice for only 1-2 days, each according to their availability. Yet it provided the foundation for development of a new clinical application.
Then I go home. Next steps are to refine the mind map, modify/update/specialise any archetypes for which we have identified new requirements and build the new ones. And in parallel start the collaborative process through a CKM project to ensure that existing and modified archetypes are ‘fit for (our project’s) purpose’, and to upload and initiate reviews on the new draft archetypes.
All work to progress these archetypes to maturity (ie aiming for clinical consensus) and then validate the templates as ready for handover to the implementers can be done online, asynchronously and at a time convenient to the clinicians work/life balance!
I live over 2000 kilometres away from these clinicians. Yet the combination of web conference and CKM enables us to operate as an ongoing collaborative team. It seems to be working well at the moment... No doubt I'll continue to learn how to do it better.
The Archetype Journey...
I'm surprised to realise I've been building archetypes for over 7 years. It honestly doesn't feel that long. It still feels like we are in the relatively early days of understanding how to model clinical archetypes, to validate them and to govern them. I am learning more with each archetype I build. They are definitely getting better and the process more refined. But we aren't there yet. We have a ways to go! Let me try to share some idea of the challenges and complexities I see…
We can build all kinds of archetypes for different purposes.
There are the ones we just want to use for our own project or purpose, to be used in splendid isolation. Yes, anyone can build an archetype for any reason. Easy as. No design constraints, no collaboration, just whatever you want to model and as large or complex as you like.
But if you want to build them so that they will be re-used and shared, then a whole different approach is required. Each archetype needs to fit with the others around it, to complement but not duplicate or overlap; to be of the same granularity; to be consistent with the way similar concepts are modelled; to have the same principles regarding the level of detail modelled; the same approach to defining scope; and of course the same approach to defining a clinical concept versus a data element or group of data elements… The list goes on.
Some archetypes are straightforward to design and build, for example all the very prescriptive and well recognised scales like the Braden Scale or Glasgow Coma Scale. These are the 'no brainers' of clinical modelling.
Some are harder and more abstract, such as those underpinning a clinical decision support system of orders and activities to ensure that care plans are carried out, clinical outcomes achieved and patients don't 'fall through the cracks' from transitions of care.
Then there are the repositories of archetypes that are intended to work as single, cohesive pool of models – each archetype for a single clinical concept that all sits closely aligned to the next one, but minimising any duplication or overlap.
That is a massive coordination task, and one that I underestimated hugely when we embarked on the development of the openEHR Clinical Knowledge Manager, and especially more recently, the really active development and coordination required to manage the model development, collaboration and management process within the Australian CKM – where the national eHealth program and jurisdictions are working within the same domain of models, developing new ones for specific purposes and re-using common, shared models for different use cases and clinical contexts.
The archetype ecosystems are hard, numbers of archetypes that need to work together intimately and precisely to enable the accurate and safe modelling of clinical data. Physical examination is the perfect example that has been weighing on my mind now for some time. I've dabbled with small parts of this over the years, as specific projects needed to model a small part of the physical exam here and there. My initial focus was on modelling generic patterns for inspection, palpation, auscultation and percussion – four well identified pillars of the art of clinical examination. If you take a look at the Inspection archetype clinicians will recognise the kind of pattern that we were taught in First Year of our Medical or Nursing degrees. And I built huge mind maps to try to anticipate how the basic generic pattern could be specialised or adapted for use in all aspects of recording the inspection component of clinical examination. Over time, I have convinced myself that this would not work, and so the ongoing dilemma was how to approach it to create a standardised, yet extraordinarily flexible solution.
Over time, I have convinced myself that this would not work, and so the ongoing dilemma was how to approach it to create a standardised, yet extraordinarily flexible solution.
Consider the dilemma of modelling physical examination. How can we capture the fractal nature of physical examination? How can we represent the art of every clinician's practice in standardised archetypes? We need models that can be standardised, yet we also need to be able to respond to the massive variability in the requirements and approach of each and every clinician. Each profession will record the same concept in different levels of detail, and often in a slightly different context. Each specialty will record different combinations of details. Specialists need all the detail; generalists only want to record the bare basics, unless they find something significant in which case they want to drill down to the nth degree. And don't forget the ability to just quickly note 'NAD' as you fly past to the next part of the examination; for rheumatologists to record a homunculus; for the requirement for addition of photos or annotated diagrams! Ha – modelling physical examination IS NOT SIMPLE!
I think I might have finally broken the back of the physical examination modelling dilemma just this week. Seven years after starting this journey, with all this modelling experience behind me! The one sure thing I have learned – a realisation of how much we don't know. Don't let anyone tell you it is easy or we know enough. IMO we aren't ready to publish standards or even specifications about this work, yet. But we are making good, sound, robust progress. We can start to document our experience and sound principles.
This new domain of clinical knowledge management is complex; nobody should be saying we have it sorted...
The White Wizard is Walking
I received my Walking Jacket at the reception desk of my Italian hotel. I'd just paid an exorbitant amount of tax in exchange for receive my jacket from the Italian Postal Service for my trusty, favourite jacket to be turned into a disruptive artwork by @ReginaHolliday. I first wore it to the Medical Informatics Europe Conference in Pisa in August 2012 and then to the ISO TC 215 meeting in Vienna the following September. I'd heard about Regina and her family's story some time before, my awareness raised purely through the twitter community, and then finding images of her 73 cents mural. I finally met her at HIC12, the Australian health informatics conference in Sydney in early August.
Regina was a keynote speaker and during her HIC address, many in the audience were clearly moved. It is the only presentation that I have seen in the health IT environment that received a standing ovation – powerful stuff. It polarised people. Most loved it and felt inspired; some thought it inappropriate in a healthIT conference – go figure!
Regina and I talked one night at dinner. She offered to paint me a jacket. I felt a bit like a fraud – I have no special patient data faux pas story to tell. My involvement in health IT stems from having a long-term engagement with the health system from the tender age of 5; about how that influencing my decision to become a doctor; and my subsequent, almost accidental, slip sideways into health informatics. Nowadays my work focus is firmly on getting health data right, working collaboratively with international clinicians to agree on common definitions about how to represent clinical content in electronic health records.
 And yet here is my jacket – a favourite that I bought way back in 2000 for my first foray out of clinical practice and into the corporate world - my first step into health informatics. I hadn't worn it for a while and Regina's painting has given it a new lease of life. It now has its own story - having travelled to the US to be painted, on to Europe to be worn for the first time in Italy and Vienna, and now back home to Australia.
And yet here is my jacket – a favourite that I bought way back in 2000 for my first foray out of clinical practice and into the corporate world - my first step into health informatics. I hadn't worn it for a while and Regina's painting has given it a new lease of life. It now has its own story - having travelled to the US to be painted, on to Europe to be worn for the first time in Italy and Vienna, and now back home to Australia.
Regina hasn't explained the image to me. I've asked … and waited. She promised to blog about it, but I think I'll be waiting a while. In her gallery of jackets that tell personal stories, mine is number 176.
So let me share what I think it portrays…
I was hit by a car when I was five years old. As a result I started my first day of school on crutches and in plaster from my waist to my right ankle – that young girl on crutches and wearing a caliper is me. Mini-me!
That accident resulted in some permanent problems and I ended up experiencing a series of operations during my childhood and early teenage years. Way too much time was spent in hospital than was healthy, but I still remember telling my orthopaedic surgeon that I wanted to be a Nurse. I remember him saying 'Rubbish. You shouldn't do that much walking. You should be a Doctor, instead"! Maybe it planted a seed. I don't remember it influencing my decision to enter medicine, but that is where I found myself. I'm not sure that as a young intern and resident years we walked less than the nurses – my memory is we never stopped running!
I practiced medicine for over 15 years, gradually side-stepping into health informatics as I joined my husband in developing, marketing, selling, supporting one of the first prescribing systems in Australia. He was the geek GP, passionate to combine his love of clinical practice with technology. I merely agreed to support him in his venture, having absolutely no idea what I was getting myself into.
That kickstarted the health informatics chapter of my life – 17 years duration to date - which has propelled my husband and myself jointly into the world of business, from cottage industry to large corporate consulting firms, and travel to some extraordinary places.
 The adult woman in Regina's image is also me – as the 'omowizard'. This has become my online persona, largely now related to Twitter and blogging. 'omowizard' originated from a love of Tolkien and seeking a Hotmail account back in 2000. Gandalf was taken, as was the 'white wizard'. So given my laundry responsibilities for my young family at the time, I became whiter than white – the Omo wizard. For those unaware, Omo is a brand of clothes washing powder that at the time claimed to wash clothes 'whiter than white'! I never dreamed anyone else would ever have to know or understand that, not even when I experimented on Twitter for the first time as @omowizard. Now it is probably too late to change :)
The adult woman in Regina's image is also me – as the 'omowizard'. This has become my online persona, largely now related to Twitter and blogging. 'omowizard' originated from a love of Tolkien and seeking a Hotmail account back in 2000. Gandalf was taken, as was the 'white wizard'. So given my laundry responsibilities for my young family at the time, I became whiter than white – the Omo wizard. For those unaware, Omo is a brand of clothes washing powder that at the time claimed to wash clothes 'whiter than white'! I never dreamed anyone else would ever have to know or understand that, not even when I experimented on Twitter for the first time as @omowizard. Now it is probably too late to change :)
In the painting I am standing in isolation on a very tall, narrow, bleak pillar. I'm not quite sure what that is representing. Some have suggested a reference to Sauron's tower in Lord of the Rings, but maybe that's too fanciful! I certainly don't have any magic powers. My youngest child informed me recently that I have a strong maternal death stare as a superpower, but I don't think that counts. Maybe it represents the approach that we have been using to standardise the clinical content for health records. It is known as openEHR and although I have been heavily involved in developing the clinical modelling side of it – building archetypes and training others. It has stood in isolation for many years and outside of the mainstream approaches to health IT, but in recent years has become recognised and is gaining increasing recognition as a significant contributor towards the goal of semantic interoperability. Only Regina knows the answer to this one!
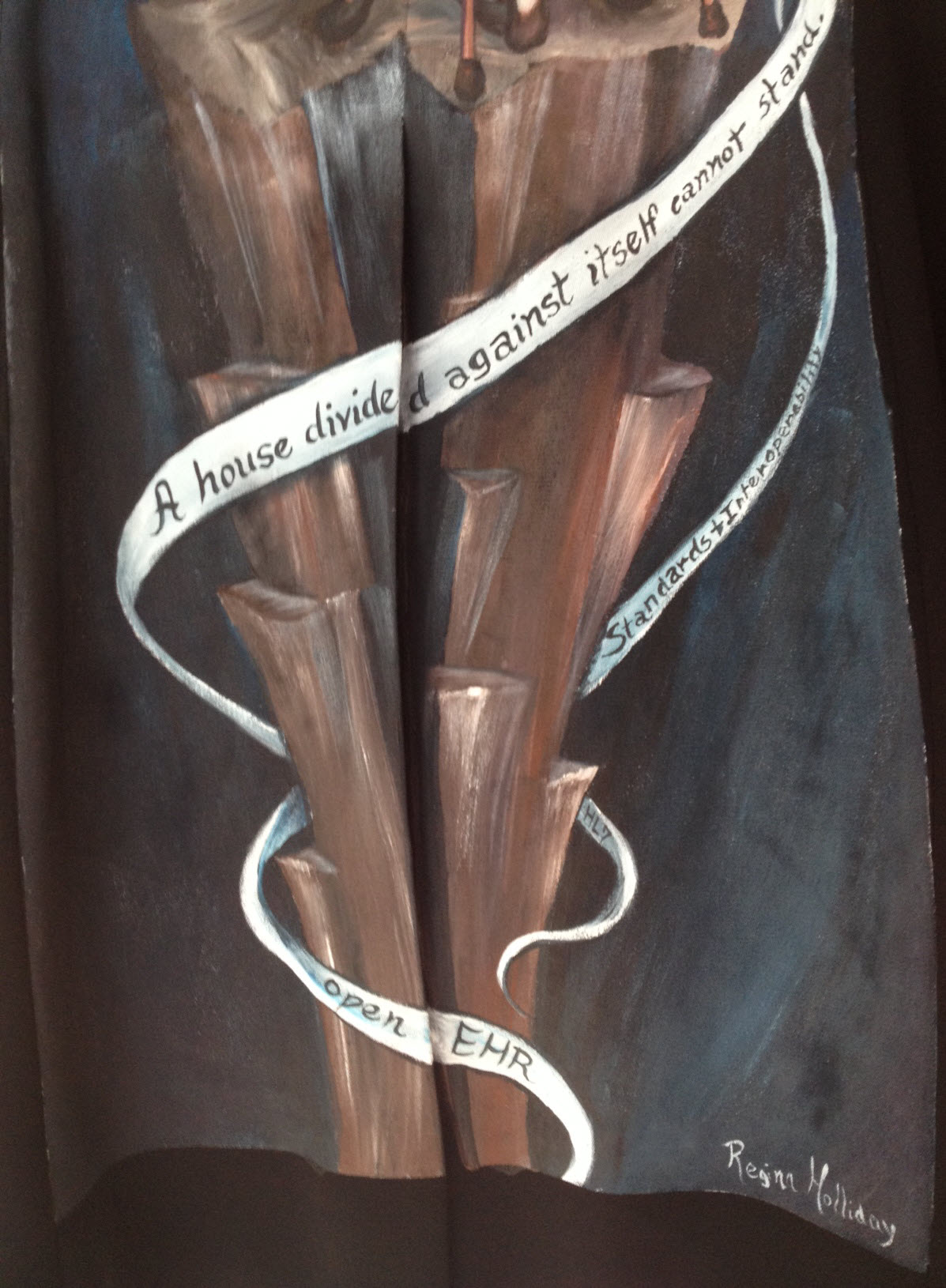 The ribbons or strands entwining around the tower are really interesting to me. The main one rippling across the tower reads: "A house divided against itself cannot stand". This appears to be a direct reference to Jesus' words in Matthew 12:25 – "He knew what they were thinking and told them, "Every kingdom divided against itself is destroyed, and every city or household divided against itself will not stand." (NIV 2012). Abraham Lincoln used the phrase in a speech to Republican candidates at the Republican State Convention on June 16, 1858 relating to the danger of slavery-based disunion. Apparently it is still used sometimes in political speeches, calling for unity and working together for a common goal.
The ribbons or strands entwining around the tower are really interesting to me. The main one rippling across the tower reads: "A house divided against itself cannot stand". This appears to be a direct reference to Jesus' words in Matthew 12:25 – "He knew what they were thinking and told them, "Every kingdom divided against itself is destroyed, and every city or household divided against itself will not stand." (NIV 2012). Abraham Lincoln used the phrase in a speech to Republican candidates at the Republican State Convention on June 16, 1858 relating to the danger of slavery-based disunion. Apparently it is still used sometimes in political speeches, calling for unity and working together for a common goal.
The lowest ribbon says simply, 'openEHR'; the one immediately to its right, 'HL7'; and just above it, 'Standards and Interoperability'.
I had described the approach that we are taking with our openEHR clinical modelling to Regina as one in which we are engaging with clinicians and domain experts to verify that the computable definitions that we are building in openEHR systems are fit for purpose. It is a collaborative approach that is crowdsourcing clinical expertise using the Clinical Knowledge Manager tool. For many years there had been little engagement with the HL7 community as a whole, although recently there appear to have been a softening of the lines of political demarcation. Those not constrained by political blinkers can see there could be significant mutual benefit from openEHR content definitions being used within HL7 constructs. Who knows if this will eventuate? And then there are other opportunities such as the CIMI and FHIR projects… Collaborating is the key.
So I interpret the ribbons yielded by the omowizard as another way of Regina calling for collaboration and collective action in healthIT. It seems that she is portraying me as a coordinator of some of the standardisation occurring in healthIT around the archetype work – using the @omowizard's twitter and blogging being one of the means to coordinate and share the passion, perhaps!
I love the painting but in trying to interpret it, it is not a comfortable image for me. I don't like being the focus. I am certainly enjoying my small bit part in the openEHR clinical modelling and health IT standards world. I have come to openEHR when it was relatively immature. We are seeing it grow and become established, but it is definitely not my idea or vision. I'm just one of number who have had the exciting opportunity of being a facilitator for something that I believe will make a difference.
I hope that when I wear this jacket it will trigger some discussions that might further progress in sharing health information and impacting the provision of health care – that is reason enough to wear it.
Thankyou, Regina. My jacket is a piece of art that is beautiful to look at; It is a powerful statement when understood in context of its origins; and is potentially a disruptive force when considered as part of the larger international Walking Gallery movement. I look forward to more opportunities to wear it at home in Australia and in my travels.
Archetype Re-use
Last Thursday & Friday @hughleslie and I presented a two day training course on openEHR clinical modelling. Introductory training typically starts with a day to provide an overview – the "what, why, how" about openEHR, a demo of the clinical modelling methodology and tooling, followed by setting the context about where and how it is being used around the world. Day Two is usually aimed at putting away the theoretical powerpoints and getting everyone involved - hands on modelling. At the end of Day One I asked the trainees to select something they will need to model in coming months and set it as our challenge for the next day. We talked about the possibility health or discharge summaries – that's pretty easy as we largely have the quite mature content for these and other continuity of care documents. What they actually sent through was an Antineoplastic Drug Administration Checklist, a Chemotherapy Ambulatory Care Nursing Intervention and Antineoplastic Drug Patient Assessment Tool! Sounded rather daunting! Although all very relevant to this group and the content they will have to create for the new oncology EHR they are building.
Perusing the Drug Checklist ifrst - it was easily apparent it going to need template comprising mostly ACTION archetypes but it meant starting with some fairly advanced modelling which wasn't the intent as an initial learning exercise.. The Patient Assessment Tool, primarily a checklist, had its own tricky issues about what to persist sensibly in an EHR. So we decided to leave these two for Day Three or Four or..!
So our practical modelling task was to represent the Chemotherapy Ambulatory Care  Nursing Intervention form. The form had been sourced from another hospital as an example of an existing form and the initial part of the analysis involved working out the intent of the form .
Nursing Intervention form. The form had been sourced from another hospital as an example of an existing form and the initial part of the analysis involved working out the intent of the form .
What I've found over years is that we as human beings are very forgiving when it comes to filling out forms – no matter how bad they are, clinical staff still endeavour to fill them out as best they can, and usually do a pretty amazing job. How successful this is from a data point of view, is a matter for further debate and investigation, I guess. There is no doubt we have to do a better job when we try to represent these forms in electronic format.
We also discussed that this modelling and design process was an opportunity to streamline and refine workflow and records rather than perpetuating outmoded or inappropriate or plain wrong ways of doing things.
So, an outline of the openEHR modelling methodology as we used it:
- Mind map the domain – identify the scope and level of detail required for modelling (in this case, representing just one paper form)
- Identify:
- existing archetypes ready for re-use;
- existing archetypes requiring modification or specialisation; and
- new archetypes needing development
- Specialise existing archetypes – in this case COMPOSITION.encounter to COMPOSITION.encounter-chemo with the addition of the Protocol/Cycle/Day of Cycle to the context
- Modify existing archetypes – in this case we identified a new requirement for a SLOT to contain CTCAE archetypes (identical to the SLOT added to the EVALUATION.problem_diagnosis archetype for the same purpose). Now in a formal operational sense, we should specialise (and thus validly extend) the archetype for our local use, and submit a request to the governing body for our additional requirements to be added to the governed archetype as a backwards compatible revision.
- Build new archetypes – in this case, an OBSERVATION for recording the state of the inserted intravenous access device. Don't take too much notice of the content – we didn't nail this content as correct by any means, but it was enough for use as an exercise to understand how to transfer our collective mind map thoughts directly to the Archetype Editor.
- Build the template.
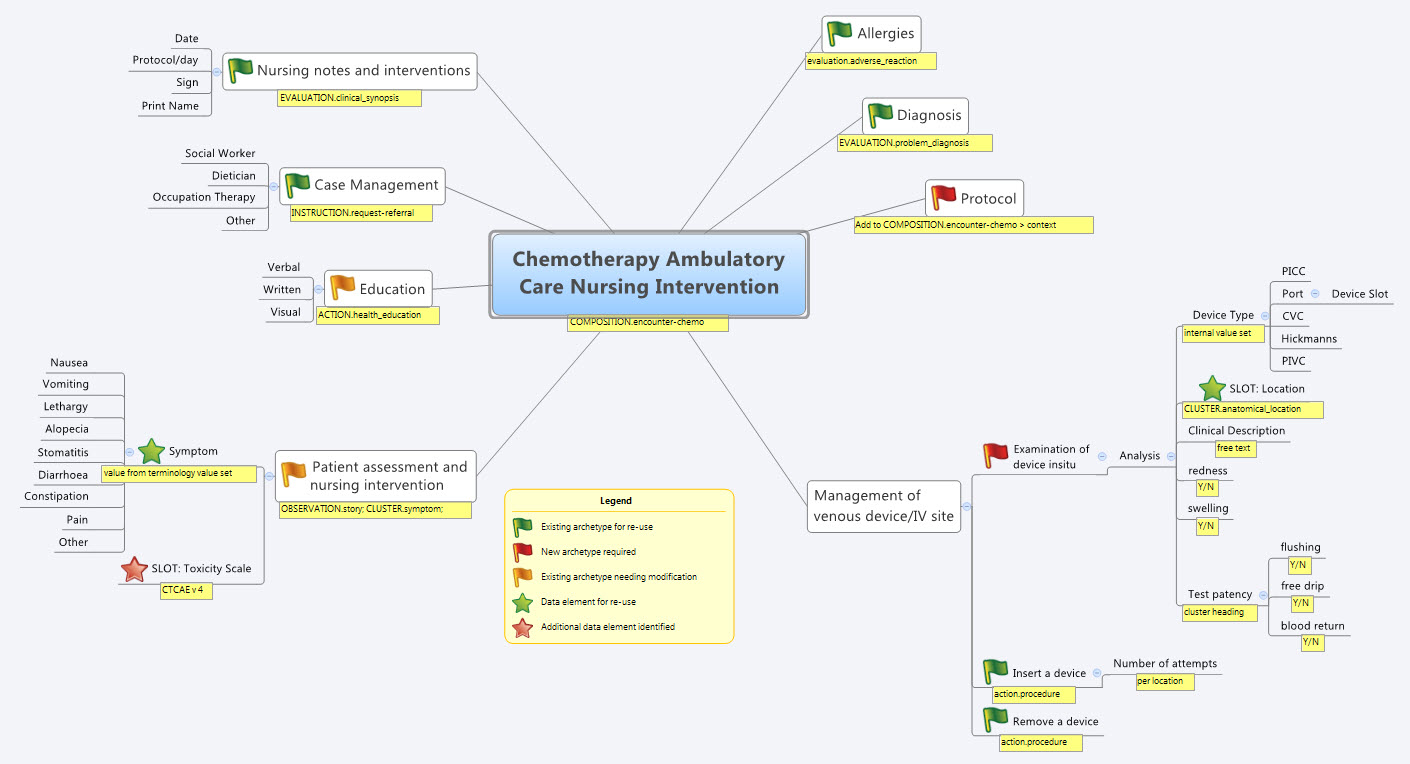
So by the end of the second day, the trainee modellers had worked through a real-life use-case including extended discussions about how to approach and analyse the data, and with their own hands were using the clinical modelling tooling to modify the existing, and create new, archetypes to suit their specific clinical purpose.
What surprised me, even after all this time and experience, was that even in a relatively 'new' domain, we already had the bulk of the archetypes defined and available in the NEHTA CKM. It just underlines the fact that standardised and clinically verified core clinical content can be re-used effectively time and time again in multiple clinical contexts.The only area in our modelling that was missing, in terms of content, was how to represent the nurses assessment of the IV device before administering chemo and that was not oncology specific but will be a universal nursing activity in any specialty or domain.
So what were we able to re-use from the NEHTA CKM?
- COMPOSITION.encounter
- EVALUATION.adverse_reaction – one instance per adverse reaction included in a adverse reaction list
- EVALUATION.clinical_synopsis
- EVALUATION.problem_diagnosis – one instance per diagnosis included in a problem list
- INSTRUCTION.request-referral – one instance per referral requested
- ACTION.health_education
- ACTION.procedure – with two instances for different purposes
…and now that we have a use-case we could consider requesting adding the following from the openEHR CKM to the NEHTA instance:
- OBSERVATION.story
- CLUSTER.symptom – with multiple instances for each symptom identified
And the major benefit from this methodology is that each archetype is freely available for use and re-use from a tightly governed library of models. This openEHR approach has been designed to specifically counter the traditional EHR development of locked-in, proprietary vendor data. An example of this problem is well explained in a timely and recent blog - The Stockholm Syndrome and EMRs! It is well worth a read. Increasingly, although not so obvious in the US, there is an increasing momentum and shift towards approaches that avoid health data lock-in and instead enable health information to be preserved, exchanged, aggregated, integrated and analysed in an open and non-proprietary format - this is liquid data; data that can flow.
The Times, They Are a-Changin’...
Channelling Bob Dylan? Not quite! But it is interesting to see some emerging HL7 and openEHR activity, at least in this little part of the world – Australia and New Zealand :) Maybe this is a model for the rest of the world - at least food for thought!
For too many long years there appears to have been a palpable barrier between the HL7 and openEHR communities. Some individuals have managed to bridge it, but there has definitely been a reluctance to engage at organisational level. It stems from before my time; I suspect vocal personalities with strong, diverging opinions were at the root. To some, it is a little like a religious argument – where "only my way is the right way"!
Be that as it may - the barrier appears to be softening and became evident to me for the first time back in January last year as I attended the HL7 meeting in Sydney. A full day openEHR workshop was presented by a diverse group of Australian companies plus NEHTA experts; Bob Dolin in attendance, amongst others. Keith Boone tweeted his initial impression of the openEHR approach after I demonstrated our tooling and then blogged about it. My thoughts were captured in my Adventures of a clinician in HL7 post.
Fast forward to 2012…
You may have seen some announcements from New Zealand. Firstly, publication in April of the Health Information Exchange Architecture Building Blocks where they specified "2.3.2 The data definitions of the Content Model shall be formulated as openEHR archetypes" within the "10040.2 HIE Content Model, a framework for the creation of a common set of logical data definitions" document.
And secondly: HL7 New Zealand and the openEHR Foundation signed a Statement of Collaboration - also announced April 2012. Now there's a headline that might have been a surprise to many – HL7 NZ & openEHR clearly intending to work closely together!
Only last Thursday Hugh Leslie & I participated in a seminar, "Bringing the Electronic Health Record to Life," organised by HL7 NZ, Health Informatics New Zealand (HINZ) and the University of Auckland. Prof Ed Hammond, 'the father of HL7', keynoted the meeting: "EHR - The Killer App". In the afternoon mini-tutorials, David Hay presented on FHIR, and Hugh, I and Koray Atalag presented a little about our openEHR work, including clinical knowledge governance and clinician engagement. Koray (a HL7 NZ member and openEHR localisation program coordinator) announced within the meeting that HL7 NZ is the likely organisation to auspice a NZ chapter of openEHR. Now that definitely has to start to change the openEHR/HL7 dynamic somewhat, even if HL7 NZ is a relatively small international affiliate :). The HL7 NZ leadership, to their absolute credit, are certainly not being constrained by any traditional 'turf wars'.
The following day, last Friday, Hugh and I presented a full day workshop on openEHR, again sponsored by HL7 NZ, HINZ and the University of Auckland. As I understand it, this was the first opportunity for the openEHR approach to be socialised with the broader healthIT community in NZ; about 25 in attendance including members of the HL7 NZ Board, vendors, and regional and HealthIT Board reps. The focus was on how openEHR could support the creation of a range of technical artefacts to meet NZ's requirements for CDA messaging (and beyond), generated from a cohesive and governed pool of clinical content models.
Interestingly we had a surprise attendee for the workshop – Ed Hammond joined us for the whole day. I won't presume to guess what Ed has taken away from the day, although he did offer up a comment to the group about the value of exploring use of archetype content directly within CDA.
Post workshop one of the attendees tweeted:
"At #HINZ #openEHR talks last 2 days. openEHR is a fantastic foundation for practical action. Left knowing steps I will take. How cools that!"
And of course, there is an HL7 AU meeting in Sydney early next week entitled "FHIR? CIMI? openEHR? What's the Future of eHealth & mHealth Standards?" The agenda:
- Keynote: Ed Hammond (again) – "FHIR, CIMI and openEHR - What's the Future for eHealth Standards?". [It will be very interesting to hear his opinion after last week's openEHR exposure.]
- Grahame Grieve: "FHIR – What is it? Why has it suddenly become so popular?"
- Hugh Leslie: "Recent developments in openEHR and CDA", and
- I'll be reporting on the CIMI project.
It would be an interesting day to be a fly on the wall! 2 HL7-ers and 2 openEHR-ers addressing an HL7 meeting - all exploring alternatives to the current approaches!
So, keep your eye on the space where HL7 intersects with openEHR – might be some interesting developments.
_______________________
Within the openEHR community, and definitely within Ocean Informatics where I work, we are certainly finding that significant interest is being certainly generated from many sources about the process of using standardised and governed openEHR clinical content as a means to generate range of technical artefacts, including CDA. The New Zealand national interest and activity is evident, as outlined above. And in addition:
- In Australia, NEHTA has piloted the use of clinician-reviewed archetypes from the NEHTA Clinical Knowledge Manager as the start point for generating a number of the PCEHR technical specifications. This work is ongoing and being extended.
- CIMI, the initiative that grew out of HL7 but is now independent, is seeking to develop an internationally agreed approach to clinical modelling and generation of multiple technical outputs. It has already agreed to utilise openEHR ADL 1.5 as its modelling formalism and is using the openEHR Reference Model as the starting point for developing a CIMI Reference Model. We watch this progress with interest.
- And Brazil's national program has recently reconfirmed its intention to commence using openEHR.
Whether the final solution is openEHR or CIMI or even something else, I think that the advent of standardised clinical models as the common starting point for generation of a range of technical outputs is upon us. Ignore it at your peril. And specifically, I would suggest that HL7 International should be considering very seriously how to embrace this new approach.
Sticking with the quasi-gospel theme, maybe it is now a bit more like Curtis Mayfield's "People Get Ready":
People get ready There's a train a-coming You don't need no baggage Just a-get on board
Let's leave our baggage behind, get on the 'train' together to collaborate and create something that transcends any health IT domain turf war! Don't get left behind...
Warts and all: Reviewing an archetype
During my visit to HIMSS12 in February, I finally met Jerry Fahrni (@JFahrni) face to face - a pharmacist and Twitter colleague I'd had 140 character conversations over some years. We'd also talked on Skype once about some of the clinical archetypes some time ago, and during our HIMSS conversation I managed to persuade him to take a look at the openEHR community's Adverse Reaction archetype and participate in the community review.
He did, and at my further request he has put ink to blog and has recorded his experience as a newbie reviewer so that others might have some sense of what completing an archetype review entails, warts and all.
Jerry's review, reproduced here:
...According to good ol’ Merriam-Webster an archetype is “the original pattern or model of which all things of the same type are representations or copies: also : a perfect example“. Simple enough, but still too vague for my brain so I went in search of a better explanation which I found at Heather’s blog – Archetypical.
According to the Archetypical site ”openEHR archetypes are computable definitions created by the clinical domain experts for each single discrete clinical concept – a maximal (rather than minimum) data-set designed for all use-cases and all stakeholders. For example, one archetype can describe all data, methods and situations required to capture a blood sugar measurement from a glucometer at home, during a clinical consultation, or when having a glucose tolerance test or challenge at the laboratory. Other archetypes enable us to record the details about a diagnosis or to order a medication. Each archetype is built to a ‘design once, re-use over and over again’ principle and, most important, the archetype outputs are structured and fully computable representations of the health information. They can be linked to clinical terminologies such as SNOMED-CT, allowing clinicians to document the health information unambiguously to support direct patient care. The maximal data-set notion underpinning archetypes ensures that data conforming to an archetype can be re-used in all related use-cases – from direct provision of clinical care through to a range of secondary uses.” That gave me a better understanding of what they were trying to do.
Anyway, when Heather asked me to review the Adverse Reaction archetype I was a little hesitant. The projects I’m asked to be involved with are typically much smaller in scale. This was something different and I felt a little intimidated. My gut reaction was to politely decline, but when someone asks you to do something face to face it makes excusing yourself for some lame reason a lot harder. So I agreed with more than a bit of trepidation.
The openEHR project utilizes a system called the Clinical Knowledge Manager (CKM). In the most basic terms, the CKM is an online content management system for all the archetypes being designed by the openEHR project, and it’s impressive. A more in depth description can be found here.
Logging into the system was simple. The email invitation I received to review the Adverse Reaction Archetype contained a link that took me to the exact location I was supposed to be. From there things got a bit more complicated. The CKM is easy enough to navigate, but the amount of information and navigational elements within the system is staggering. It took me a while to figure out exactly what I was supposed to do. Once I figured it out I was able to quickly go through the archetype, read what other comments people had made and make a couple of minor notes myself. One thing I could never completely figure out was how to save my work in the middle and continue later. Sounds simple enough, but for whatever reason it just wasn’t obvious to me. I ended up powering through my “review” in one extended session because I was afraid I’d lose my place. The archetype itself was impressive. It’s clear from the information and detail that people have spent a lot of time and effort developing the adverse reaction archetype. There’s no question that a lot of great minds had been involved in this work. The definition made sense as did the data that was being collected and presented. The archetype offered flexibility for information gathering that included the simplest form of adverse reaction to complex re-exposure and absolute contraindication notation (this is sorely missing in many systems I’ve used over my career). Overall I had little insight to offer during the review, only a couple of minor comments.
I’d say the entire process was pretty straightforward with some minor complications. Like everything else I’m sure the process would get easier over time and multiple uses.
Thanks Jerry. Your independent and honest opinion is much valued. Perhaps next time... !! (Just joking)
CIMI... one of many crossroads
Grahame Grieve posted CIMI at the Crossroads recently. I can't disagree with a lot of the content, but maybe I'm a bit more of an optimist as I draw some slightly different conclusions. Grahame is totally right about what it has achieved so far:
- a significant membership roll that has never been achieved before
- a significant agreement of an initial approach to clinical models - a primary formalism of ADL 1.5/AOM with a commitment to support transformation to isosemantic UML models in a spirit of inclusivity and harmonisation.
And as he points out, the notion that the modelling methodology was chosen independently of the Reference Model is somewhat disconcerting.
"...the decision to choose ADL/AOM as the methodology, while deferring the choice of reference model. While I understood the political reality of this decision, choosing an existing methodology (ADL/AOM) but not the openEHR reference model committed CIMI to building at least a new tooling chain, a new community, and possibly a new reference model.
The cost of this is high; so high that the opportunity created by the foundation of CIMI may likely founder if we see another attempt to reinvent the health IT wheel, yet again.
There are many opinions, and everyone at the CIMI table has their own bias, history, experience. Organisational and personal investment in each existing solutions are high. No one wants to throw away their efforts and 'start again'; everyone wants their work to be the successful and sustained.
The CIMI community do need to make an objective decision if it is to move forward. It may not be result which wins a popularity contest. It is very likely that some members will walks away and keep working as they always have; maybe intending to return when a more mature solution is on offer.
In his paragraph on the pros and cons of openEHR, Grahame very eloquently states:
This is the first choice: pick the least worst established clinical modelling paradigm.
:)
"Least worst" - Thanks Grahame! You could turn that around: the 'best' available so far, where there is no perfect solution!
But it's not a bad principle - to take the least worst and make it better!
The chair of the openEHR board, Sam Heard proposed the following to the openEHR community back in October 2011:
“If the CIMI group chooses to use ADL as the formalism then the openEHR community is prepared to explore the Foundation governance arrangements with the CIMI group and align the two efforts using the structures that are mutually agreed.
Changes to ADL and the openEHR Reference Model may be part of the process to meet the collective needs, and alignment of the shared RM and a reviewed RM for ISO 13606 would also be a major goal. ADL 1.5 would be submitted to ISO as part of this alignment.”
Seems sensible to me - start with a robust candidate and modify/enhance it to meet the collective needs. The latest version of the openEHR RM is clearly one candidate. It has evolved significantly from the 2005 version which forms the basis of ISO 13606. Given that ISO 13606 (parts 1-5) is due for revision this year, perhaps we have a great opportunity for harmonisation. The openEHR community is already starting to develop a proposal for the revision, but a greater achievement would be to align all of these efforts into a new 13606/openEHR/CIMI specification.
This is a difficult task that we are trying to solve. We know that because it has not been solved before.
This is definitely not the first crossroad that CIMI has encountered - don't underestimate the effort that has brought the group to this point - and it will definitely not be the last. What will determine success is keeping the end goal front and centre in CIMI's decision-making; cutting ruthlessly through the political and personal agendas; putting pragmatism ahead of perfection; and a willingness to compromise in order to move forward.
It may not be possible. It could be a hell of a ride. I still think it has the potential make a hell of a difference.
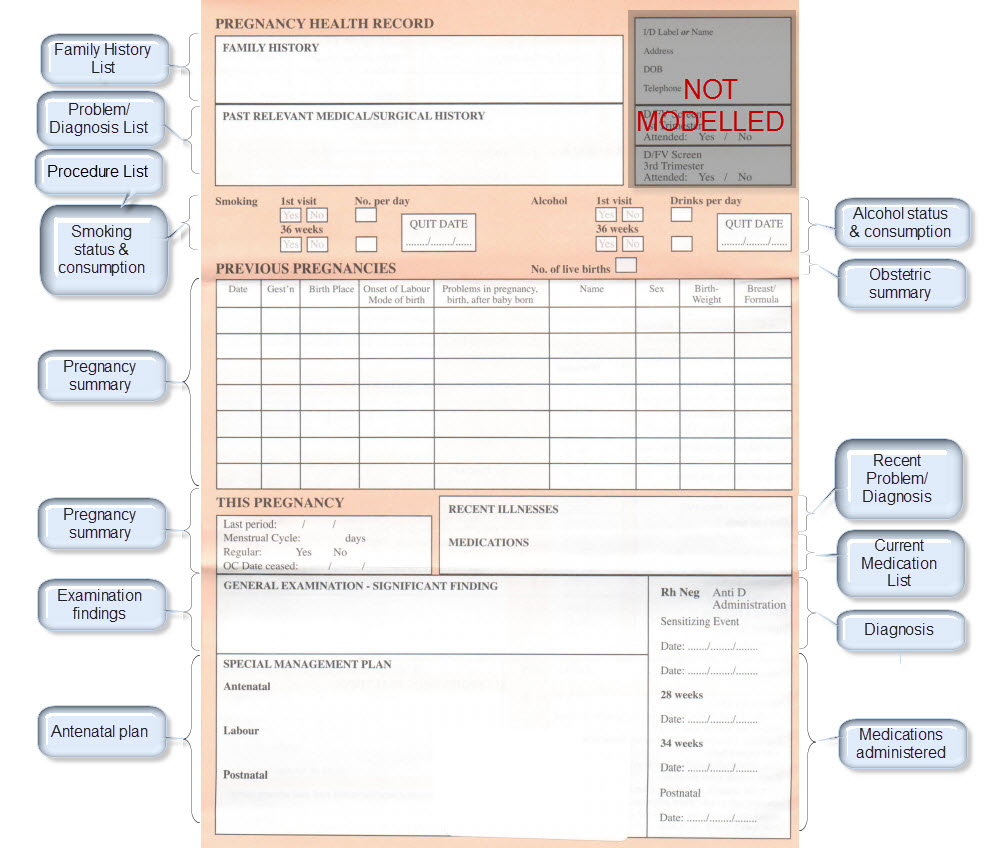
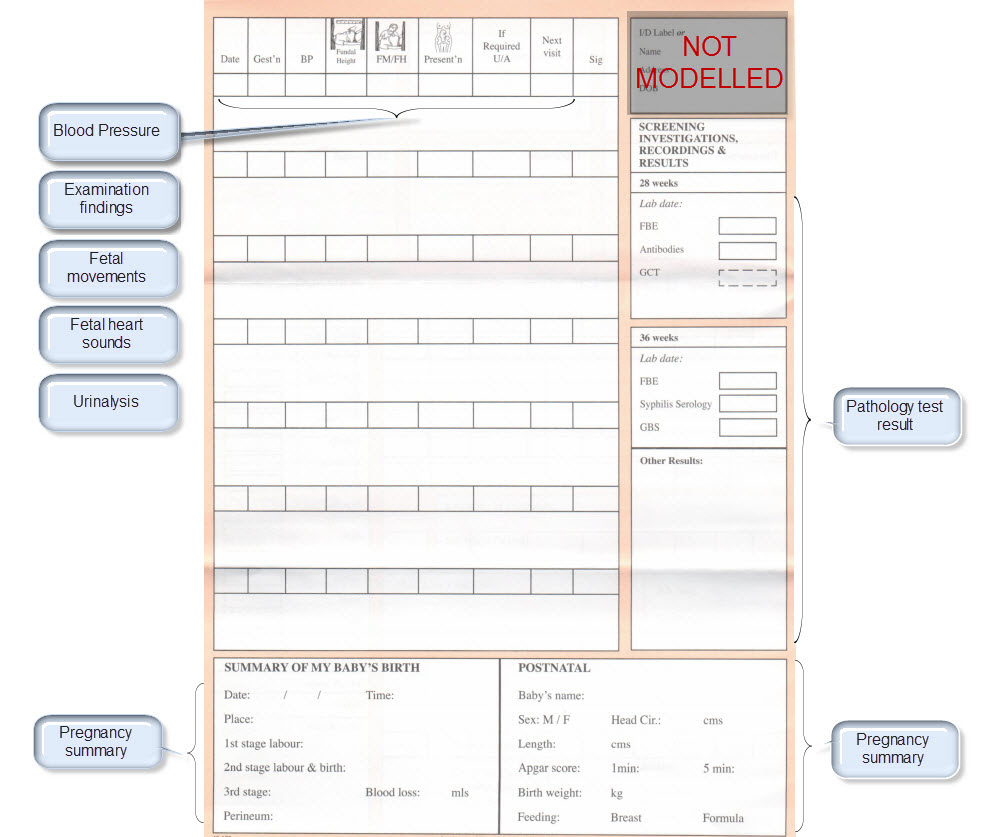
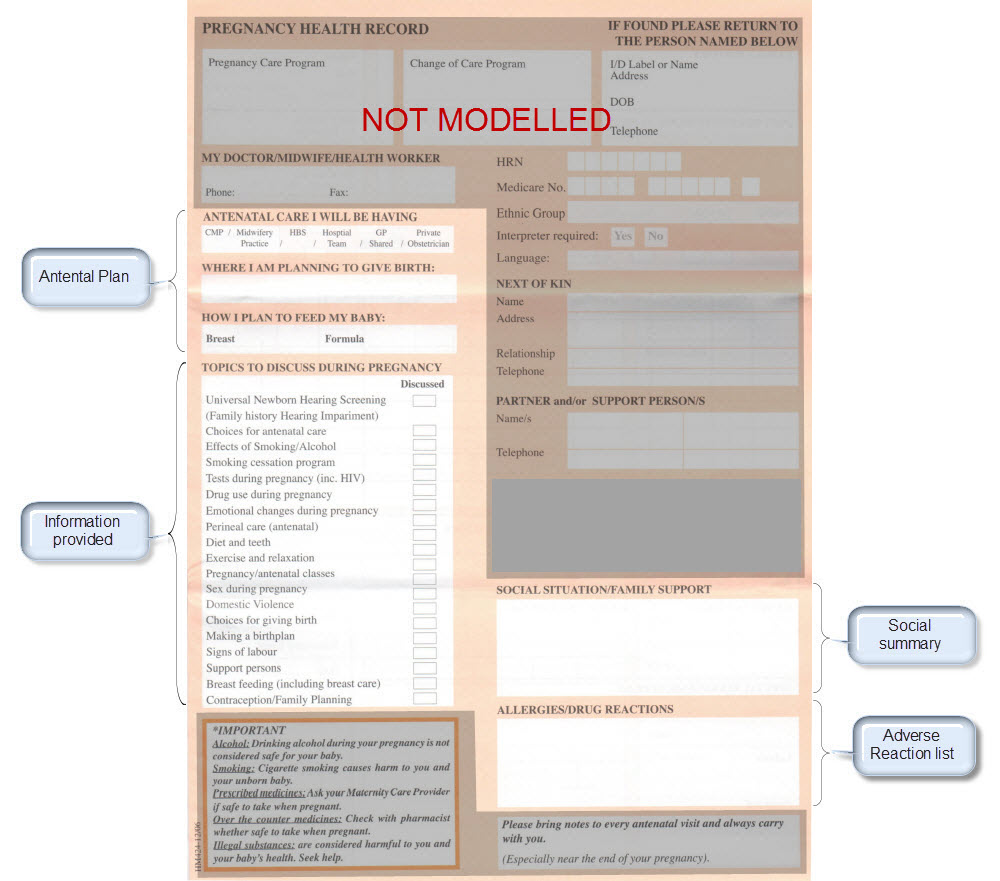
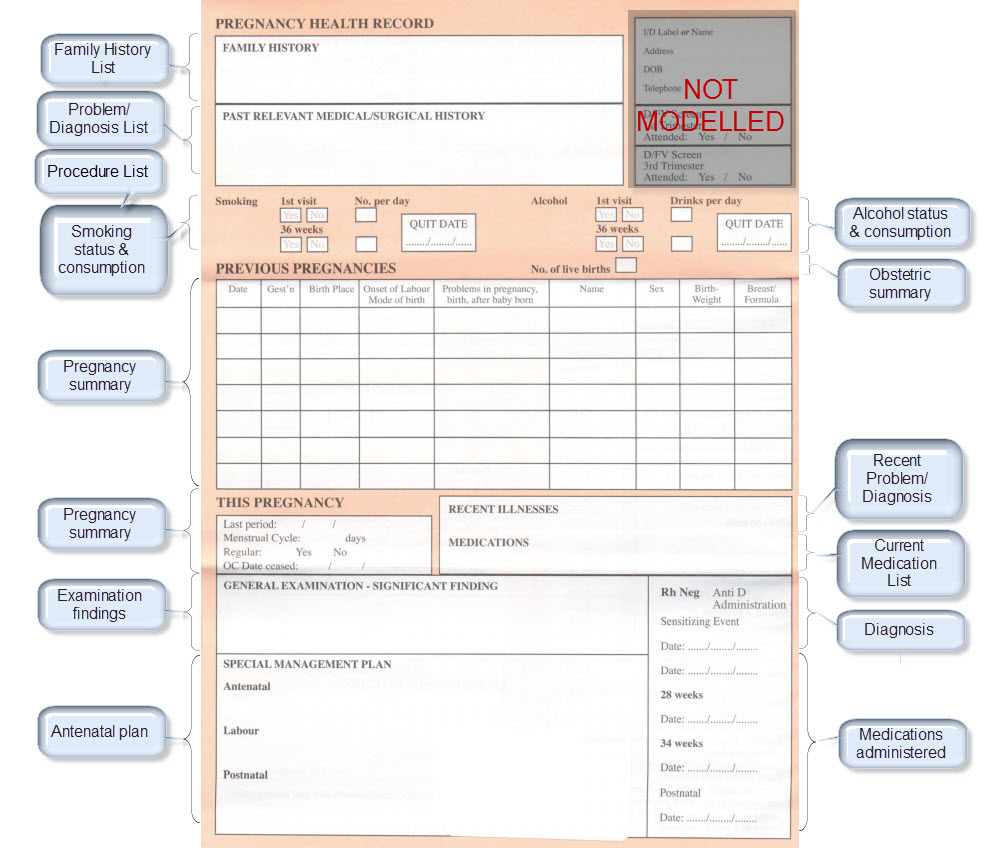
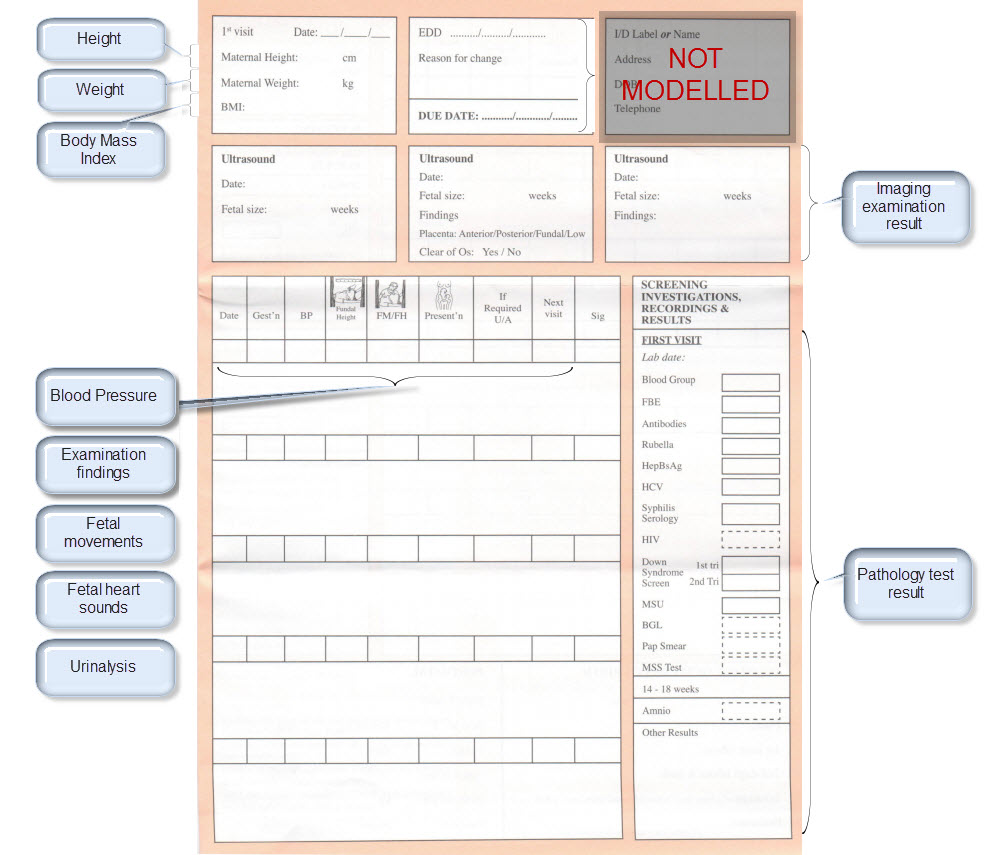
Modelling pregnancy
Step 2: Map clinical concepts to archetypes
Map them to existing archetypes or determine which new ones we need. Determine the state of the existing archetypes – do we need to modify or enhance with additional requirements? Consider all possible use cases for each archetype – the end result will be better if we can be as inclusive as possible for all clinical scenarios.
The archetypes identified for this Pregnancy record are:
| Clinical Concept | Comment |
Corresponding archetype concept name NOTE: is linked to the actual archetype in a CKM instance |
| Antenatal Plan | An overarching plan for the patient's antenatal care | Antenatal Plan <INSTRUCTION.antenatal_plan> |
| Information Provided | Details of each piece of health education information discussed or provided to patient | Information Provided <ACTION.health_education> |
| Social Summary | Social Summary <EVALUATION.social_summary> | |
| Adverse Reaction List | Adverse Reaction list is made up of multiple Adverse Reaction entries | Adverse Reaction <EVALUATION.adverse_reaction> |
| Family History List | Family History list is made up of multiple Family History entries | Family History <EVALUATION.family_history> |
| Diagnosis | Problem lists, whether current or past are made up of multiple Problem/Diagnosis entries – the same data pattern will be used in all instances | Problem/Diagnosis <EVALUATION.problem_diagnosis> |
| Problem/Diagnosis List | ||
| Recent Problem/Diagnosis List | ||
| Procedure list | Procedure list is made up of multiple Procedure entries | Procedure <ACTION.procedure> |
| Smoking consumption | Tobacco use <OBSERVATION.substance_use-tobacco> | |
| Alcohol consumption | Alcohol consumption <OBSERVATION.substance_use-alcohol> | |
| Obstetric Summary | Obstetric summary <EVALUATION.obstetric_summary> | |
| Pregnancy Summary | An evolving summary of key data about a single pregnancy – either current or past | Pregnancy summary <EVALUATION.pregnancy_summary> |
| Examination Findings | Examination Findings <OBSERVATION.exam> Examination of the uterus <CLUSTER.exam-uterus> Examination of the fetus <CLUSTER.exam-fetus> | |
| Current Medication List | Medication list is made up of multiple Medication instruction entries | Medication instruction <INSTRUCTION.medication> |
| Medication administered | Medication action <ACTION.medication> | |
| Height | Height/Length <OBSERVATION.height> | |
| Weight | Body weight <OBSERVATION.body_weight> | |
| Body Mass Index | Body Mass Index <OBSERVATION.body_mass_index> | |
| Blood Pressure | Blood Pressure <OBSERVATION.blood_pressure> | |
| Fetal Movements | Fetal Movements <OBSERVATION.fetal_movements> | |
| Fetal heart sounds | Heart rate and rhythm <OBSERVATION.heart_rate> | |
| Urinalysis | The pattern for urinalysis is identical to the pathology test results, and in some cases will be performed in the lab, so the same pattern will be used | Pathology test result <OBSERVATION.pathology_test> |
| Pathology Test results | ||
| Ultrasound results | Imaging examination result <OBSERVATION.imaging_exam> |
KEY: Pink archetype names indicate those that are early drafts. Green archetype names indicate those that are reasonably mature – through previous reviews within CKM Red archetype names indicate those yet to be developed.
Step 3: CKM Review
Within CKM each archetype will undergo review rounds by a range of clinicians, terminologists, software engineers, informaticians and other interested experts. The purpose of each review round will be to fine-tune each archetype so that it meets the requirements for each stakeholder group.
CKM Videos:
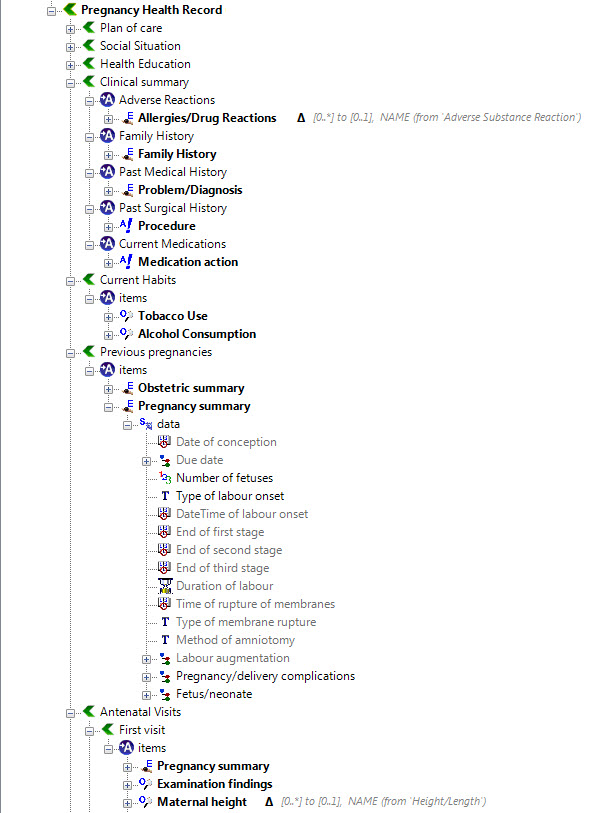
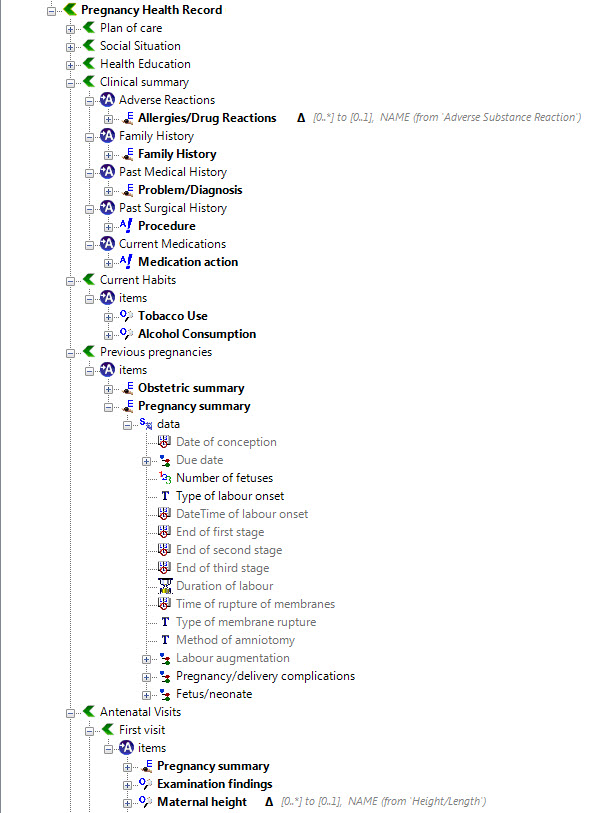
Step 4: Create an openEHR template
Once community consensus is reached within CKM, the archetypes will be aggregated and constrained in a template to accurately meet the specific use-case requirements for this particular Pregnancy Health Record. Each bold, black heading in the the following screenshot represents an archetype. The Pregnancy Summary archetype has been opened up to see the details. Black text indicates data elements that will be utilised in this use case; grey text indicates inactive data elements.
Other groups may use the same archetypes aggregated in a different order and constrained in a different way to represent their version of the Pregnancy Health Record. As the data in both Pregnancy Records is being recorded according to the same pattern, dictated by the underlying archetype, the information can be exchanged without ambiguity or loss of meaning.