 'Severity' is a pretty simple clinical concept, isn't it?
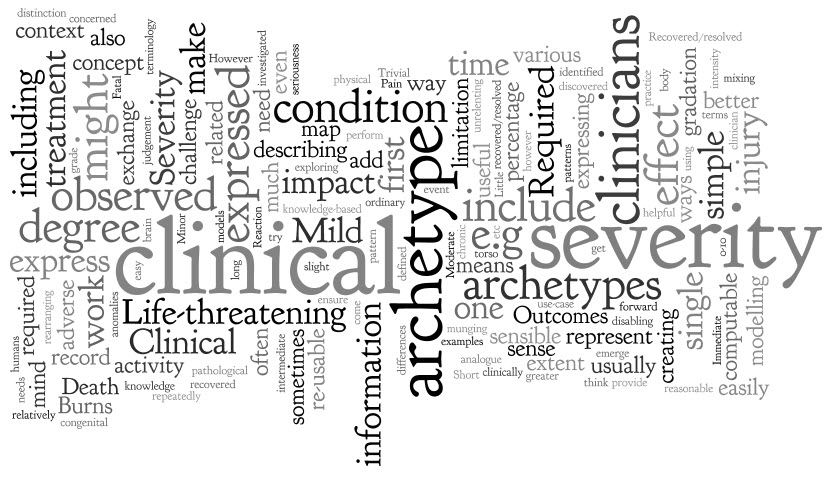
I thought so too until I first sat down to create a single, re-usable archetype to represent 'Severity'. I soon discovered that I had significantly underestimated it - the challenge was greater than appeared at first glance.
'Severity' is a pretty simple clinical concept, isn't it?
I thought so too until I first sat down to create a single, re-usable archetype to represent 'Severity'. I soon discovered that I had significantly underestimated it - the challenge was greater than appeared at first glance.
The archetype development process is usually relatively straight forward - a brain dump of all related information into a mind map, followed by rearranging the mind map until sensible patterns emerge. They usually do, but not this time.
However, the more I investigated and researched, the more I could see that clinicians express severity in a variety of ways, sometimes mixing and 'munging' various concepts together in such a way that humans can easily make sense of it, but it is much harder to represent in a way that is both clinically sensible and computable.
The simple trio of 'Mild', 'Moderate' and 'Severe' is commonly used as a gradation to express the severity of a condition, injury or adverse event. Occasionally these are defined for a given condition or injury, however most often these are subjective and there should be concern that one clinician's mild might be another's moderate. Some also include intermediate terms, such as 'Mild-to-moderate' and 'Moderate-to-severe', but one has to begin to be concerned if these more subtle differences make the judgement even more unreliable, especially if we need to exchange information between systems.
Others add 'Trivial' – is this less than 'Mild'? By how much? Is there a true gradation here? And what of 'Extreme'? Still others add 'Life-threatening' and 'Death' – but are these really expressing severity? Or are they expressing clinical impact or even an outcome?
When exploring severity I found examples of severity expressed by clinicians in many ways. This list is by no means exhaustive:
- Pain – expressed as intensity, often including a visual analogue scale as a means to record it ie rate from 0-10
- Burns – describing percentage of body involved e.g. >80% burns
- Burns – describing the depth of burn by degree e.g. first degree
- Perineal tears – describe the extent and damage by degree – e.g. second degree tear
- Facial tic – expressed in using frequency e.g. occasional through to unrelenting
- Cancer – expressed as a grade, clinical or pathological
- Rash – extent or percentage of a limb or torso covered.
- Minor or major
- Mild, disabling life-threatening
- Relative severity – better, worse etc
- Functional impact – ordinary activity, slight limitation, marked limitation, inability to perform any physical activity
- Short or long term persistence
- Acute or chronic
In practice, clinicians can work interchangeably with any of these expressions and make reasonable clinical sense of it. The challenge when creating archetypes, and other computable models, is to ensure that clinicians can express what they need in a health record, exchange that information safely with other clinicians, allow for knowledge-based activities such as decision support.
In addition, there also needs to be a clear distinction between 'severity' and other, related qualifiers that provide additional context about 'seriousness' of the condition, injury or adverse reaction. These sometimes get thrown into the mix as well, including:
- Clinical impact (or significance);
- Clinical treatment required; and
- Outcomes.
Clinical impact/significance might include:
- None - No clinical effect observed
- Insignificant - Little noticeable clinical effect observed.
- Significant - Obvious clinical effect observed
- Life-threatening - Life-threatening effect observed
- Death – Individual died.
Immediate clinical treatment required might include:
- No treatment
- Required clinician consultation
- Required hospitalisation
- Required Intensive Care Unit
Outcomes might include:
- Recovered/resolved
- Recovering/resolving
- Not recovered/resolved
-
Fatal
Then there are those that recovered or the condition resolved but there were other sequelae such as congenital anomalies in an unborn child...
Severity ain't simple.
Over time, and repeatedly returning to it when modelling it in various archetypes including Adverse Reaction and Problem/Diagnosis, I've come to the conclusion that I don't think it is useful or helpful for us to model 'severity' in a single, re-usable archetype. It seems to work better as a single qualifier element within archetypes – then we can bind it in to terminology value sets that are useful for that specific archetype concept and for the use-case context.
When a clinical knowledge pattern is easily identified, creating an archetype is easy - the archetype almost writes itself! So over time I've learned not to try to force the modelling. Some archetypes 'work'; some, like this one, just don't.
