Incoherence is not ideal, but it is a realistic part of any work such as we are doing within the openEHR community. Transparency and openness can mitigate some of the incoherence. Within a transparent, governed and collaborative environment incoherence and apparent conflict can be recognised and leveraged constructively to improve the quality of archetypes.
A little dance, clap & cheer
Case Study: Clinical Engagement
Bridging the gap between the clinical experts and software engineers involved in eHealth projects is well known for being difficult and frustrating for both sides. The openEHR methodology is having great success in bringing the non-technical clinicians along with us on the clinical modelling journey.
Brazilian EHR innovation, powered by openEHR
Fractal exam findings II
The scope and diversity of clinical content in the physical examination domain is huge and complex, with different clinicians requiring different levels of detail. We have developed a base pattern for recording physical examination findings, knowing that the concept-specific detail within each model will need be added as backwardly compatible revisions of these archetypes. In this way they will evolve in an organic way to suit clinical requirements, but within a tightly governed environment.
Fractal exam findings I
The extremely complex nature of the clinician's physical examination is an obvious benchmark test for the capability of any modelling paradigm. If you can't model the clinical requirement for something as fundamental, yet frustratingly diverse as physical examination, then you need to go back to the drawing board until it works. This post outlines our journey...
Archetype patterns
The challenge for FHIR: meeting real world clinician requirements
With the increasing burden of technical engagement resulting from the incredible expectations generated by FHIR globally, perhaps the clinical content specification should be outsourced to... the clinicians first of all, ensuring that the clinical content can be represented in a technical format for implementation.
EHR building blocks
For many years I have borrowed an analogy using Lego building blocks rather than the notion of generic 'shapes' - that if we get the foundation building blocks agreed and fit for use in our EHRs (ie clinical archetypes), then they can be re-used in multiple contexts and combined in any permutation or combination to represent the clinical documentation that we need.
openEHR & FHIR
Take off the low-res sunglasses
Clinical modelling, openEHR style
The outcome of a program of coordinated clinical content standardisation provides a long term and sustainable national approach to developing, maintaining and governing jurisdictional health data specifications. It can form the backbone for a national health data strategy and is a key way to ensure that clinicians contribute their expertise to jurisdictional eHealth programs.
The unknown substance conundrum...
Therapeutic Precautions are the 'new black'!
Clinical modelling around the concepts of warnings, alerts and notifications is incredibly complex and each of the terms are loaded with confusion. It is not going to be easy to navigate this area and achieve a common understanding that will underpin information models for sensible and cross paradigm decision support.
Inaugural joint archetype review by HL7 & openEHR!
#Uncomplexication of Clinical Infostructure
My presentation delivered remotely from Australia to the Arctic Conference on Dual-Model based Clinical Decision Support & Knowledge Management in Tromsø, Norway today.
The Archetype 'Elevator Pitch'
Know your data?
Recently I was reminded of some work we did a number of years ago. It involved a large research database, painstakingly collected over 20 years. The data was defined across a number of specialisations within a single clinical domain and represented in 83 data dictionaries stored in an Excel spreadsheet.
Data was collected based on a series of questionnaires, and we were told that successive data custodians had, true to human nature, made slight tweaks and updates to the questionnaires on multiple occasions. The data collected was actually evolving!
The only way to view the data was to open each of the 83 spreadsheets, painstakingly, one by one.
We were engaged to create archetypes to represent both the legacy data and the data that the research organisation wished to standardise to take forward.
So the activity of converting these data dictionaries - firstly to archetypes for each clinical concept, and then representing each data dictionary as a template - resulting in considerable insight into the quality and scope of the data that hadn't been available previously.
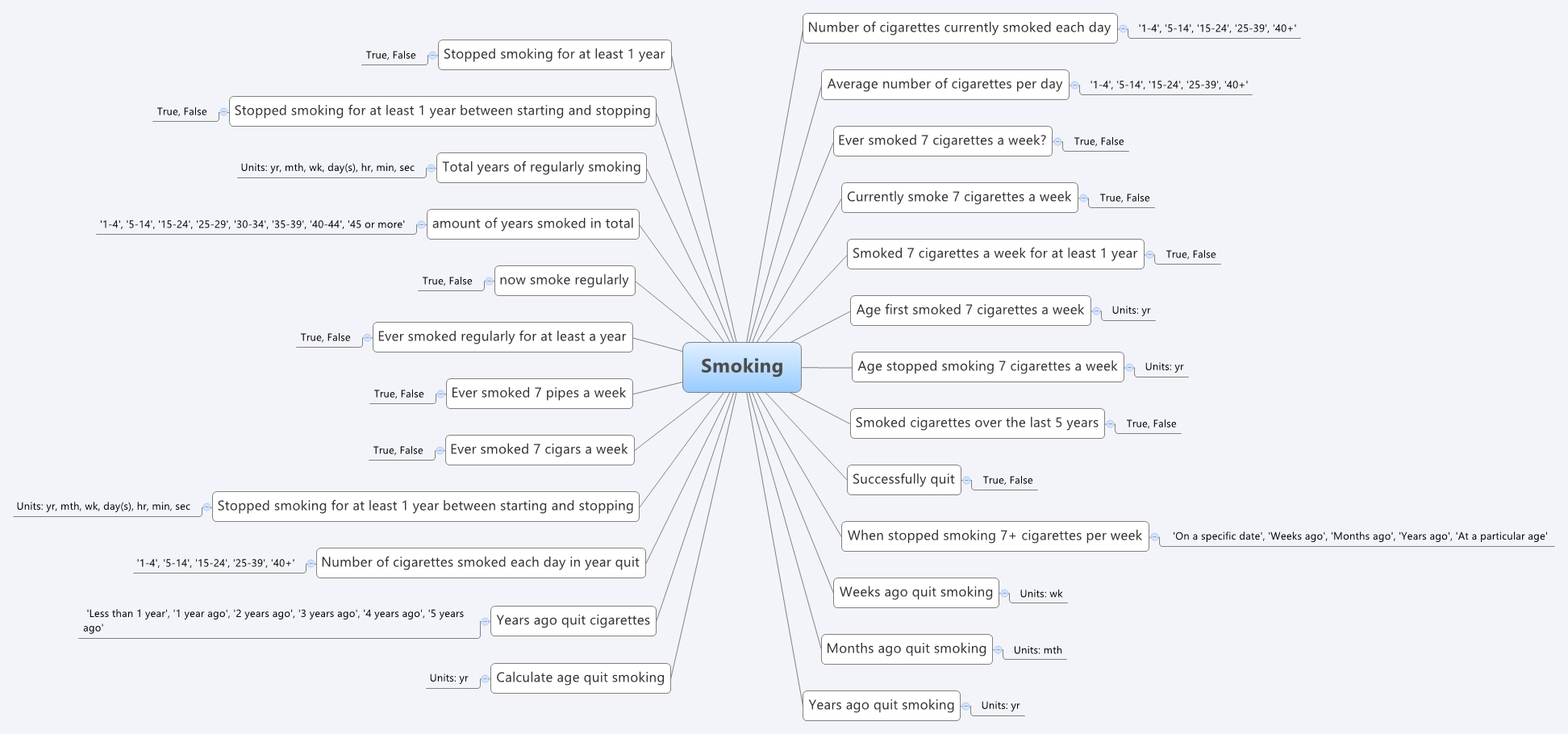
For example, the mind map below is an aggregation of the various ways that questions were asked about the topic of smoking.
 Interestingly, what it showed was that no one individual in the organisation had full oversight of the detailed data in all of the data dictionaries.The development of the archetypes effectively provided a cross section of the data focusing on commonality at a clinical concept level and revealed insights into the whole data collection that was a major surprise to the research organisation. It triggered an internal review and major revision of their data.
Interestingly, what it showed was that no one individual in the organisation had full oversight of the detailed data in all of the data dictionaries.The development of the archetypes effectively provided a cross section of the data focusing on commonality at a clinical concept level and revealed insights into the whole data collection that was a major surprise to the research organisation. It triggered an internal review and major revision of their data.
Some of the issues apparent in this mind map are:
- A number of questions have been asked in slightly different ways, but with slight semantic variation, thus creating the old 'apples' vs 'pears' problem when all we wanted was a basket of apples;
- Often the data is abstracted and recorded in categories, rather than recording the actual, valuable raw data which could be used for multiple purposes, not just he purpose of the rigid categories;
- Some questions have 'munged' two questions together with a single True/False answer, resulting in somewhat ambiguous data; and
- Some questions are based on fixed intervals of time.
No doubt you will see other issues or have more variations of your own you could share in your systems.
And we have repeatedly seen a number of our clients undergo this same process, where archetypes help to reveal issues with enormously valuable data that had previously been obscured by spreadsheets and the like. The creation of archetypes and re-use of archetypes as consistent patterns for clinical content has an enormous positive impact on the quality of data that is subsequently collected.
And while harmonisation and pattern re-use within one organisation or project can be hard enough, standardisation between organisations or regions or national programs or even internationally has further challenges. It may take a while to achieve broader harmonisation but the benefits of interoperability will be palpable when we get there.
In the meantime the archetypes are a great way to trigger the necessary conversations between the clinicians, domain experts, organisations, vendors and other interested parties - getting a handle on our data is a human issue that needs dialogue and collaboration to solve.
Archetypes are a great way to get a handle on our data.
Preventing health data 'black holes'!
It really is not surprising that scientific data is disappearing all the time. But, oh, think of the value of this data - in terms of cost and knowledge. Irreplaceable. The original article from Smithsonian.com is here: The vast majority of raw data from old scientific studies may now be missing.
Some excerpts:
A new survey of 20-year-old studies shows that poor archives and inaccessible authors make 90 percent of raw data impossible to find.
...
When a group of researchers tried to email the authors of 516 biological studies published between 1991 and 2011 and ask for the raw data, they were dismayed to find that more 90 percent of the oldest data (from papers written more than 20 years ago) were inaccessible. In total, even including papers published as recently as 2011, they were only able to track down the data for 23 percent.
...
"Some of the time, for instance, it was saved on three-and-a-half inch floppy disks, so no one could access it, because they no longer had the proper drives," Vines says. Because the basic idea of keeping data is so that it can be used by others in future research, this sort of obsolescence essentially renders the data useless.
...
And preserving data is so important, it's worth remembering, because it's impossible to predict in which directions research will move in the future.
Seems to me that the openEHR approach to data definitions is an excellent candidate for preventing the health data 'black hole' too!
Non-proprietary, open data specifications are a key component for future-proofing irreplaceable clinical and research data.
Archetypes/DCMs MIA in SDOs
Curious to note that there is very little apparent interest in detailed clinical information models (DCMs) of any brand or flavour in the major Standards Development Organisations (SDO's) - they are effectively Missing In Action when compared to the likes of CDA and IHE profiles. The ISO 13972 DCM specification took a long and tortuous time to travel through the ISO TC 215 processes. Engagement with 13972 during its development, and from what I can observe now it is on the verge of publication has been rather sparse. A further piece of work is now starting in ISO regarding quality criteria for DCMs but it also seems to be struggling to find an audience that understands it, or even cares.
I don't quite understand why the concept of DCMs has not been a big ticket item on the radar of the SDOs for a long time as it is a major missing piece of any standards-based framework. Groups like CIMI are raising awareness, alongside the openEHR work, so momentum is gathering, but for some reason it seems to keep a very understated profile compared to new opportunities like FHIR in HL7.
The work of messages, documents, profiles and terminologies are clearly important for interoperability, but standardisation of clinical content models working closely with terminologies can potentially make the work required to develop messages, documents, and profiles orders of magnitude easier.
Let me test a metaphor on you. Think of each message, document or profile as a sentence and each archetype or DCM as a word, a building block that is one component of each sentence. By focussing on the building a specific sentence, we are working backwards by trying to determine the components, and the outcome is still just that single sentence. However if we start by standardising the words/archetypes, then once they are stable it is relatively simple to construct not only one sentence for a specific purpose, but the potential is a much greater output in which many more additional sentences can be created using a variety of words in different combinations. If we manage the words (archetypes) as core building blocks and get them right, then we allow a multitude of possible sentences (messages/documents/profiles) to proliferate.
The ‘brand’ of archetype/DCM solution does not concern me so much as raising awareness that clinician-led, standardised clinical content is a significant missing and overlooked piece of the international eHealth foundations puzzle.
