 Clinicians, have you ever had a look at the data structures underpinning your EHR - the models of clinical content? If you don't understand the principles of what your data structure is then your EHR may not do, or ever be able to do, all the things you need it to do to record your clinical notes. You need a sense of what is 'under the bonnet' and what its capabilities are.
Take Blood Pressure as an example. It is probably the most easily understood clinical concept to both clinicians and patients. We clinicians tend to think of it as a very simple measurement to record on paper, and we expect our EHR applications to do it in a similar way.
Clinicians, have you ever had a look at the data structures underpinning your EHR - the models of clinical content? If you don't understand the principles of what your data structure is then your EHR may not do, or ever be able to do, all the things you need it to do to record your clinical notes. You need a sense of what is 'under the bonnet' and what its capabilities are.
Take Blood Pressure as an example. It is probably the most easily understood clinical concept to both clinicians and patients. We clinicians tend to think of it as a very simple measurement to record on paper, and we expect our EHR applications to do it in a similar way.
So let's brainstorm about what we need to record blood pressure. The typical primary care provider such as a General Practitioner or Nurse will record the Systolic and Diastolic pressures, plus maybe a blood pressure cuff size if it is different to the 'normal' cuff, and position of the patient if recording a postural drop. This is straightforward, 'bread and butter' stuff for clinicians.
So the base data requirements are:
- Systolic – a quantity that is a pressure, measured in millimeters of mercury (mmHg)
- Diastolic – ditto
- Cuff size – most will measure using a 'normal' adult cuff, recording a size only if they use a larger or smaller cuff.
- Position – most patients in primary care will be sitting; most in hospital will be reclining
While this may cater for the large majority of our BP measurements, there are other less common situations where it is critical that BP be recorded appropriately and in context. So we need a data specification that also caters for the following situations where BP is measured, such as:
- The cardiologist or exercise physiologist may need additional data about the level of exertion for use in stress testing or research. A BP measured at rest needs to be interpreted differently to that recorded after jogging for 10 minutes.
- Recording a series of BP readings over a 24 hour period to determine the 24 hour average, plus knowing the patient's concurrent sleep status – this is now regarded as key diagnostic criteria for diagnosis of hypertension in Europe.
- Measuring data from home BP machines – many of these actually record the Mean Arterial Pressure and use an algorithm to determine the Systolic/Diastolic readings displayed.
- Automatic BP measuring every 5 minutes during surgery or an admission to Intensive Care by 'the machine that goes beep'.
- Paramedics taking a measurement of a trapped patient at the scene of an car accident.
Other questions might be clinically significant in some circumstances include:
- What Korotkoff sound was used?
- What about the implications for paediatric measurement?
- Where was the measurement taken? Which limb? Finger vs upper arm?
- How was it taken – auscultation; palpation, machine; or invasive?
- What about pregnant women who need to have their BP measured with lateral tilt to get a true reading – do we need to record that detail?
It may be very important to have this information recorded in some situations.
Maybe blood pressure is maybe not so simple, after all.
Clinicians understand clinical nuances well, recording the contextual variations appropriately in paper records – in fact it is so ingrained that it is almost done on autopilot. The problem arises in trying to get computers to do the same thing – to record simply in the usual circumstances but be able to cope with the complex and detailed where it is critically needed.
So, we need to have some understanding about the capabilities of our EHR systems. Most systems only cater for little beyond the basic four requirements. Yet most of these additional requirements that we have identified are useful or necessary at other times to ensure unambiguous BP recording.
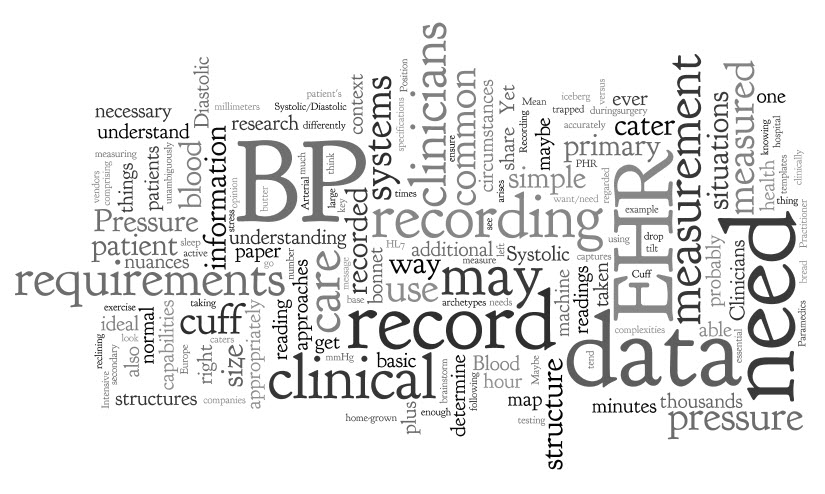
The mind map at left captures the basic versus the 'ideal' requirements. The 'ideal list may seem excessive to some. Yet if our EHR system could cater for this, then we could record all nuances of BP accurately and share them unambiguously if they share the same underlying structure - primary care to secondary care; PHR to EHR to research; patient to clinicians. So then, the 'art of the EHR' is to present the right amount of information and the right context to the clinician to let them record what they need - not too much for the common simple BP reading, but more when necessary.
Here we have started to explore the tip of the iceberg – the content scope of one common clinical measurement. The essential message here is that we clinicians need to have some understanding of what is 'under the bonnet' of our EHR systems. What may be adequate for the commonest situation is not necessarily enough for recording the complexities of clinical care.
Part II starts to explore clinician engagement in content models...

